By Susi Hately, B.Sc. Kinesiology, C-IAYT Yoga Therapist
There are all sorts of theories on improving movement which will help people to reduce pain, and improve performance. They all work, for a lot of people, most of the time.
Where all of us fall into a trap is when we get stuck on the theory that works the majority of time. Because of the success, our minds fall into a template mode that says “this is what is done for this condition, or, for this movement problem”. This can happen not only for us as the providers of care, but as clients too. The thinking becomes rigid, almost religious. When the inevitable happens – ie the theory doesn’t work in a situation – we become stuck. Because of our template mode way of thinking, we can’t see what is “actually” going on, and our eyes become “shaded” from reality.
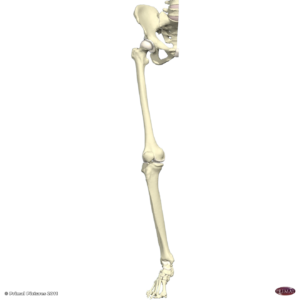
I see this a lot with weak glutes. The common refrain is people have weak glutes because they are sitting all the time. However, I have seen people who have occupations that require no sitting at all, or very minimal sitting and their glutes are not firing properly. I also see people who sit a tonne, and their glutes are firing really well. So, it isn’t just about sitting. It’s also not just about standing with poor posture. Sure those are contributory factors, but if those two scenarios were the actual issue than there would be many, many more people with weak glutes, and that is not what I am seeing or nor is it what I am hearing from other practitioners who work in different subsets of rehabilitation.
So what to do? How can we get out of template mode and learn to see more clearly?
Instead of drilling into an answer, ask a question. What else is going on in this person’s body that is leading to the current situation? As it relates to the glutes, the question might be, what else is going on in this person’s body that is leading to the glutes not engaging properly?
To answer this question as a care provider, you will not be required to look in a book, or register for another class promoting another theory. You will need to look at your client and actually see what is going on.
To answer this question as a client, you don’t need to necessarily dump the person who is providing you care, you simply need to notice what is going on in your own body. Not your friend’s body who apparently has the same condition.
What you will find is that the answer is different depending on the person. For some, there is a real rigidness in the tissue under the lower ribs, and when released, the glutes automatically begin to engage properly. Or, the rib cage begins to brace part way through the movement and if movement only happens as far as there is no bracing, the glutes begin to work better. Other people hold their jaw tight. Others overuse their outer calf or their pelvic floor instead of their glutes. Others need to release through their lateral line, or have to relearn how to twist properly.
The key is there isn’t one answer, and truly the patterns of limitation are endless. The key is to be attentive and simply watch your client and then act based on what you see. Or, if you are the client, as you are attentive to your own self moving, you can then make a change.
What I love about this way of thinking is it encompasses pretty much every movement theory out there. When you are actually watching someone, when you are being attentive to yourself and what you are seeing is a contributor (notice I didn’t use the word causal), then you will see more clearly which tool, which theory would be most appropriate at a given time. This gives you much more clarity and versatility with helping your client or yourself. And, it is a way more fun process for solving problems.
Here is another added bonus:
For the client – As you become more attentive, you become more aware, and you can integrate that awareness. As you do, you will move better, you will feel better, your pain will go down and the opportunities and freedom will go up. You will begin to see possibility again for your life. Why? Because you can’t change anything you aren’t aware of.
For the health provider – You will be empowering your own client to be attentive and integrate their awareness so that they take what you are teaching them and really apply it. This approach, while challenging at first, truly makes our job that much more fun. Rather than being the person who the client relies on for “fixing them”, the relationship becomes one of trusted advisor – helping to refine the client’s best awareness for greater and greater gains.
The bottom line to consider over the next couple of weeks – When you are seeing that something isn’t happening as it should, ask “what else is going on?”
Have fun with this.
Change is possible. For everyone – including you.
Have a great time exploring.
Susi